Neurofibromatosis type 1
Updated: 2024-09-10
Overview
Neurofibromatosis type 1 (NF1) is a genetic condition that causes changes in skin pigment and tumors on nerve tissue. Skin changes include flat, light brown spots and freckles in the armpits and groin. Tumors can grow anywhere in the nervous system, including the brain, spinal cord and nerves. NF1 is rare. About 1 in 2,500 is affected by NF1.
The tumors often are not cancerous, known as benign tumors. But sometimes they can become cancerous. Symptoms often are mild. But complications can occur and may include trouble with learning, heart and blood vessel conditions, vision loss, and pain.
Treatment focuses on supporting healthy growth and development in children and early management of complications. If NF1 causes large tumors or tumors that press on a nerve, surgery can reduce symptoms. A newer medicine is available to treat tumors in children, and other new treatments are being developed.
Symptoms
Neurofibromatosis type 1 (NF1) usually is diagnosed during childhood. Symptoms are seen at birth or shortly afterward and almost always by age 10. Symptoms tend to be mild to moderate, but they can vary from person to person.
Symptoms include:
- Flat, light brown spots on the skin, known as cafe au lait spots. These harmless spots are common in many people. But having more than six cafe au lait spots suggests NF1. They often are present at birth or appear during the first years of life. After childhood, new spots stop appearing.
- Freckling in the armpits or groin area. Freckling often appears by ages 3 to 5. Freckles are smaller than cafe au lait spots and tend to occur in clusters in skin folds.
- Tiny bumps on the iris of the eye, known as Lisch nodules. These nodules can't easily be seen and don't affect vision.
- Soft, pea-sized bumps on or under the skin called neurofibromas. These benign tumors usually grow in or under the skin but can also grow inside the body. A growth that involves many nerves is called a plexiform neurofibroma. Plexiform neurofibromas, when located on the face, can cause disfigurement. Neurofibromas may increase in number with age.
- Bone changes. Changes in bone development and low bone mineral density can cause bones to form in an irregular way. People with NF1 may have a curved spine, known as scoliosis, or a bowed lower leg.
- Tumor on the nerve that connects the eye to the brain, called an optic pathway glioma. This tumor usually appears by age 3. The tumor rarely appears in late childhood and among teenagers, and almost never in adults.
- Learning disabilities. It's common for children with NF1 to have some trouble with learning. Often there is a specific learning disability, such as trouble with reading or math. Attention-deficit/hyperactivity disorder (ADHD) and speech delay also are common.
- Larger than average head size. Children with NF1 tend to have a larger than average head size due to increased brain volume.
- Short stature. Children who have NF1 often are below average in height.
When to see a doctor
See a healthcare professional if your child has symptoms of neurofibromatosis type 1. The tumors are often not cancerous and are slow growing, but complications can be managed. If your child has a plexiform neurofibroma, a medicine is available to treat it.
Causes
Neurofibromatosis type 1 is caused by an altered gene that either is passed down by a parent or occurs at conception.
The NF1 gene is located on chromosome 17. This gene produces a protein called neurofibromin that helps regulate cell growth. When the gene is altered, it causes a loss of neurofibromin. This allows cells to grow without control.
Risk factors
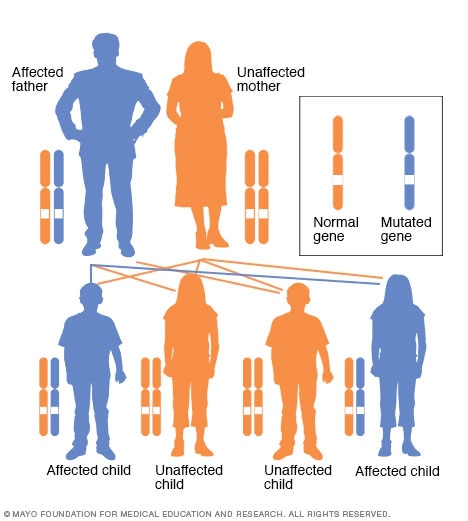
Autosomal dominant inheritance pattern
In an autosomal dominant disorder, the changed gene is a dominant gene. It's located on one of the nonsex chromosomes, called autosomes. Only one changed gene is needed for someone to be affected by this type of condition. A person with an autosomal dominant condition — in this example, the father — has a 50% chance of having an affected child with one changed gene and a 50% chance of having an unaffected child.
The biggest risk factor for neurofibromatosis type 1 (NF1) is a family history. For about half of people who have NF1, the disease was passed down from a parent. People who have NF1 and whose relatives aren't affected are likely to have a new change to a gene.
NF1 has an autosomal dominant inheritance pattern. This means that any child of a parent who is affected by the disease has a 50% chance of having the altered gene.
Complications
Complications of neurofibromatosis type 1 (NF1) vary, even within the same family. Generally, complications occur when tumors affect nerve tissue or press on internal organs.
Complications of NF1 include:
- Neurological symptoms. Trouble with learning and thinking are the most common neurological symptoms associated with NF1. Less common complications include epilepsy and the buildup of excess fluid in the brain.
- Concerns with appearance. Visible signs of NF1 can include widespread cafe au lait spots, many neurofibromas in the facial area or large neurofibromas. In some people this can cause anxiety and emotional distress, even if they're not medically serious.
- Skeletal symptoms. Some children have bones that didn't form as usual. This can cause bowing of the legs and fractures that sometimes don't heal. NF1 can cause curvature of the spine, known as scoliosis, that may need bracing or surgery. NF1 also is associated with lower bone mineral density, which increases the risk of weak bones, known as osteoporosis.
- Changes in vision. Sometimes a tumor called an optic pathway glioma develops on the optic nerve. When this happens, it can affect vision.
- Increase in symptoms during times of hormonal change. Hormonal changes associated with puberty or pregnancy might cause an increase in neurofibromas. Most people who have NF1 have healthy pregnancies but will likely need monitoring by an obstetrician who is familiar with NF1.
- Cardiovascular symptoms. People who have NF1 have an increased risk of high blood pressure and may develop blood vessel conditions.
- Trouble breathing. Rarely, plexiform neurofibromas can put pressure on the airway.
- Cancer. Some people who have NF1 develop cancerous tumors. These usually arise from neurofibromas under the skin or from plexiform neurofibromas. People who have NF1 also have a higher risk of other forms of cancer. They include breast cancer, leukemia, colorectal cancer, brain tumors and some types of soft tissue cancer. Screening for breast cancer should begin earlier, at age 30, for women with NF1 compared to the general population.
- Benign adrenal gland tumor, known as a pheochromocytoma. This noncancerous tumor produces hormones that raise your blood pressure. Surgery often is needed to remove it.
Diagnosis
To diagnose neurofibromatosis type 1 (NF1), a healthcare professional begins with a review of your personal and family medical history and a physical exam.
Your child's skin is checked for cafe au lait spots, which can help diagnose NF1.
If other tests are needed to diagnose NF1, your child may need:
- Eye exam. An eye exam can reveal Lisch nodules, cataracts and vision loss.
- Imaging tests. X-rays, CT scans or MRIs can help identify bone changes, tumors in the brain or spinal cord, and very small tumors. An MRI might be used to diagnose optic gliomas.
- Genetic tests. Genetic testing for NF1 can help support the diagnosis. Genetic tests also can be done in pregnancy before a baby is born. Ask a member of your healthcare team about genetic counseling.
For a diagnosis of NF1, at least two symptoms of the condition must be present. A child who has only one symptom and no family history of NF1 is likely to be monitored for any other symptoms. A diagnosis of NF1 is usually made by age 4.
Treatment
There isn't a cure for neurofibromatosis type 1 (NF1), but symptoms can be managed. Generally, the sooner someone is under the care of a specialist trained in treating NF1, the better the outcome.
Monitoring
If your child has NF1, often yearly age-appropriate checkups are recommended to:
- Check your child's skin for new neurofibromas or changes in existing ones.
- Check for signs of high blood pressure.
- Check your child's growth and development. This includes measuring height, weight and head circumference to compare to growth charts for children who have NF1.
- Look for signs of early puberty.
- Look for any skeletal changes.
- Check your child's learning development and progress in school.
- Get a complete eye exam.
Contact your healthcare team right away if you notice any changes in symptoms between visits. Many complications of NF1 can be treated effectively if therapy starts early.
Medicine
Selumetinib (Koselugo) is a treatment approved by the U.S. Food and Drug Administration for plexiform neurofibroma in children. The medicine can shrink the size of a tumor. Clinical trials of similar medicines are currently being done for children and adults.
Surgery and other procedures
Surgery to remove tumors may be needed to treat serious symptoms or complications of NF1. Symptoms can be relieved by removing all or part of tumors that are compressing nearby tissue or damaging organs.
Cancer treatment
Cancers related to NF1 are treated with standard cancer therapies, such as surgery, chemotherapy and radiation therapy. Early diagnosis and treatment are the most important factors for a good outcome.
Potential future treatments
Researchers are testing gene therapies for neurofibromatosis type 1 (NF1). Potential new treatments could include replacing the NF1 gene to restore the function of neurofibromin.
Coping and support
Caring for a child with a condition such as neurofibromatosis type 1 (NF1) can be a challenge. But many children with NF1 grow up to live healthy lives with few, if any, complications.
To help you cope:
- Find a healthcare professional you can trust and who can coordinate your child's care with other specialists. The Children's Tumor Foundation has an online tool to help you find a specialist in your area.
- Join a support group for parents who care for children who have NF1, ADHD, special needs or lifelong illnesses.
- Accept help for daily needs such as cooking, cleaning or caring for your other children or simply to take a needed break.
- Seek academic support for children who have learning disabilities.
Preparing for an appointment
You may be referred to a doctor who specializes in brain and nervous system conditions, known as a neurologist.
It's a good idea to be well prepared for your appointment. Here's some information to help you get ready and know what to expect.
What you can do
- Write down a list of concerns, making a note of when you first noticed them.
- Bring a complete medical and family history with you if your healthcare professional doesn't already have it.
- Write down key personal information, including any major stresses or recent life changes.
- Make a list of all medicines, vitamins or supplements that you or your child is taking.
- Bring photographs of any family members — living or deceased — who may have had similar symptoms.
- Write down questions to ask your healthcare professional.
Your time during your appointment is limited. Preparing a list of questions can help you make the most of your time. List your questions from most important to least important in case time runs out. For neurofibromatosis, some basic questions to ask include:
- Do you suspect neurofibromatosis type 1?
- What tests do you recommend?
- What treatments are available?
- How should the condition be monitored for changes?
In addition to the questions that you've prepared, don't hesitate to ask other questions that occur to you.
What to expect from your doctor
You're likely to be asked a number of questions. Being ready to answer them may allow time later to cover other points you want to address. Your healthcare professional may ask:
- When did you first notice symptoms? Have they changed over time?
- Is there a family history of neurofibromatosis type 1?